Natural killer cells dressed to kill cancer cells
New research: A new study may potentially enable scientists to provide cancer immunotherapy that is cheaper, faster and more manageable.
New work by researchers with laboratories at Oslo Cancer Cluster Incubator may help to dramatically improve a T cell-based immunotherapy approach so that it can benefit many more patients.
T cell assassins
T cells are the professional killers of the immune system – they have a unique capability to specifically recognize ‘foreign’ material, such as infected cells or cancer cells. This highly specific recognition is achieved through receptors on the surface of T cells, named T cell receptors (TCRs). Once its receptor recognizes foreign material, a T cell becomes activated and triggers the killing of the infected or cancerous cell.
Adoptive cell therapy
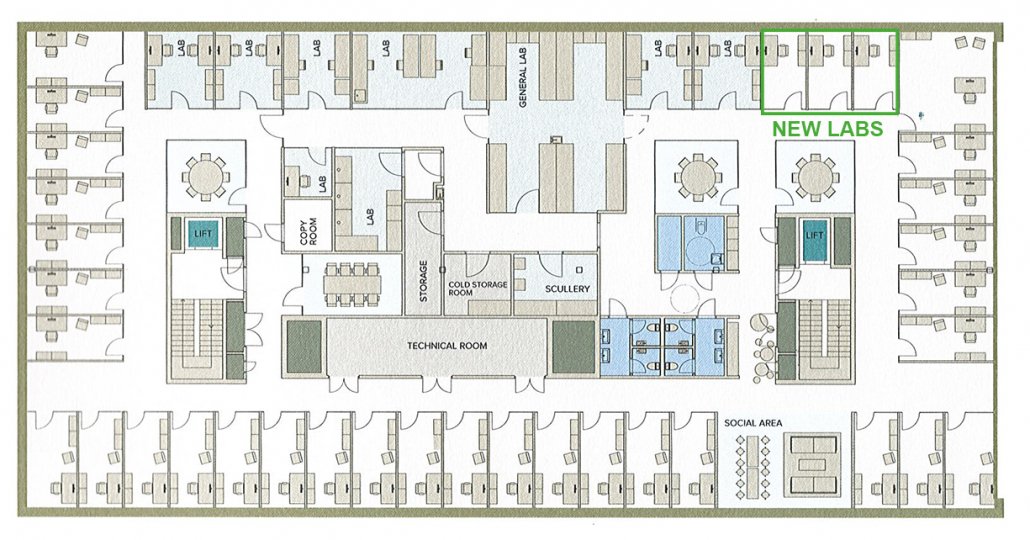
Unfortunately, many cancers have adapted fiendish ways to avoid recognition and killing by T cells. To combat this issue, an immunotherapy approach known as adoptive cell therapy (ACT) has been developed in recent years. One such ACT approach is based on the injection of modified (or ‘re-directed’) T cells into patients. The approach is further explained in the illustration below.
The left side of the illustration shows how redirected T-cell therapy involves:
1) Harvesting T cells from a cancer patient
2) Genetic manipulation of T cells to make them express an ideal receptor for recognizing the patient’s cancer cells
3) Growing T cells in culture to produce high cell numbers
4) Treating patients with large quantities of redirected T cells, which will now recognize and kill cancer cells more effectively
An alternative approach
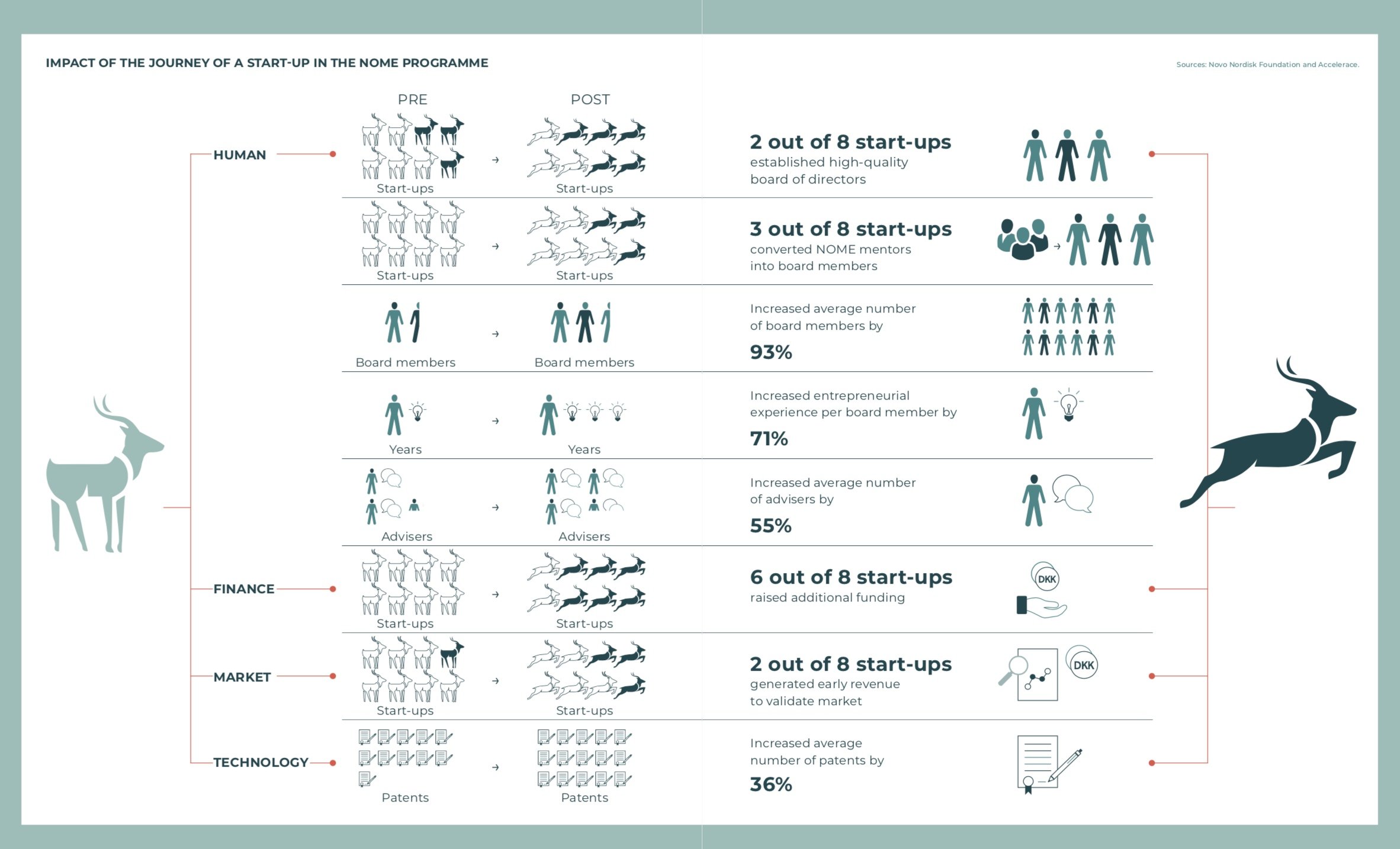
Adoptive T cell therapy has delivered very encouraging results for some cancer patients, but its application on a larger scale has been limited by the time consuming and costly nature of this approach. In addition, the quality of T cells isolated from patients who have already been through multiple rounds of therapy can sometimes be poor.
Researchers have long searched for a more automated form of adoptive cell therapy that would facilitate faster and more cost-effective T cell-based cancer immunotherapy.
One approach that has seen some success involves the use of different immune cells called Natural Killer cells – NK cells in brief.
Despite their great potential, NK cells have unfortunately not yet been proven to provide a successful alternative to standard T cell-based cancer immunotherapy. One major reason for this may be that, because NK cells do not possess T cell receptors, they are not very effective at specifically detecting and killing cancer cells.
Cells dressed to kill
The group led by Dr. Sébastien Wälchli and Dr. Else Marit Inderberg at the Department of Cellular Therapy aimed to address this issue and improve NK cell-based therapies.
They reasoned that by editing NK cells to display anti-cancer TCRs on their cell surface they could combine the practical benefits of NK cells with the potent cancer killing capabilities of T cells. This is shown in the right hand side of the illustration above.
The researchers found that by simply switching on the production of a protein complex called CD3, which associates with the TCR and is required for T cell activation, they could indeed induce NK cells to display active TCRs. These ‘TCR-NK cells’ acted just like normal T cells, including their ability to form functional connections to cancer cells and subsequently mount an appropriate T cell-like response to kill cancer cells.
This was a surprising and important finding, as it was not previously known that NK cells could accommodate TCR signaling.
This video shows TCR-NK cell-mediated killing of cancer cells in culture. The tumour cells are marked in green. Tumour cells that start dying become blue. The overlapping colours show dead tumour cells.
The researchers went on to show that TCR-NK cells not only targeted isolated cancer cells, but also whole tumours.
The method was proven to be effective in preclinical studies of human colorectal cancer cells in the lab and in an animal model. This demonstrates its potential as an effective new form of cancer immunotherapy.
Paving the way
Lead researcher Dr. Nadia Mensali said:
“These findings pave the way to the development of a less expensive, ready-to-use universal TCR-based cell therapy. By producing an expansive ‘biobank’ of TCR-NK cells that detect common mutations found in human cancers, doctors could select suitable TCR-NK cells for each patient and apply them rapidly to treatment regimens”.
Whilst further studies are needed to confirm the suitability of TCR-NK cells for widespread treatment of cancer patients, the researchers hope that these findings will be the first step on the road towards off-the-shelf immunotherapy drugs.
- Read the whole research paper at Science Direct. The paper is called “NK cells specifically TCR-dressed to kill cancer cells”.
- The researchers behind the publication consists of Nadia Mensali, Pierre Dillard, Michael Hebeisen, Susanne Lorenz, Theodossis Theodossiou, Marit Renée Myhre, Anne Fåne, Gustav Gaudernack, Gunnar Kvalheim, June Helen Myklebust, Else Marit Inderberg, Sébastien Wälchli.
- Read more about research from this research group in this article from January.
- Read more about Natural Killer cells in this Wikipedia article.