Personalising breast cancer screening in Norway
Are polygenic risk scores the key to personalising cancer prevention in Norway?
Imagine that your saliva can reveal your personal risk for developing certain diseases. Think about the possibilities of detecting cancer at an early stage, preventing serious disease and saving lives. This is what polygenic risk score (PRS) tests are all about.
The AnteNOR project has investigated how such a test for breast cancer can be implemented in the Norwegian healthcare system. In a recent seminar at Oslo Cancer Cluster Innovation Park, researchers and experts met to present the results and discuss the way forward.
Watch the seminar here:
Analysing Norwegian data
Eivind Hovig, Professor at the Centre for Bioinformatics at the University of Oslo, and group leader at Institute for Cancer Research, Oslo University Hospital, has investigated the performance of breast cancer polygenic risk score in the Norwegian population.
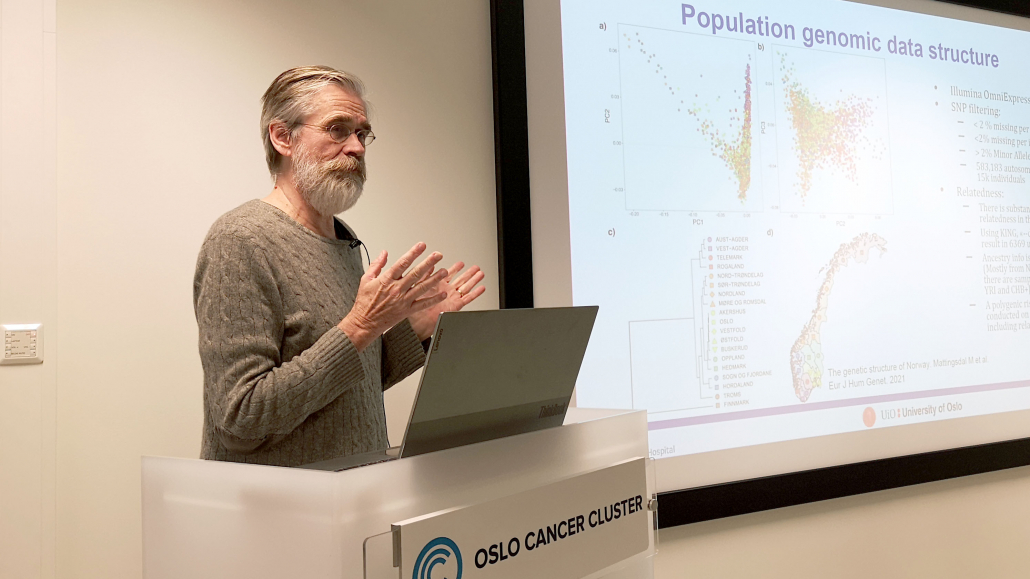
Eivind Hovig, Professor at the Centre for Bioinformatics at the University of Oslo, and group leader at Institute for Cancer Research, Oslo University Hospital. Photo: Sofia Linden / Oslo Cancer Cluster.
Denise O’Mahony, researcher at the Department of Medical Genetics, Institute of Medical Genetics at University of Oslo, supplemented Hovig’s presentation. Her research group has among other things analysed the distribution of polygenic risk scores in Norwegian data compared to Estonian data.
“By the age of 49 we see a total of 182 women that have a higher risk than the median absolute risk at 50, which is the age that women enter screening, therefore indicating the benefit of incorporating the PRS in clinical practice,” commented O’Mahony.

Denise O’Mahony, researcher at the Department of Medical Genetics, Institute of Medical Genetics at University of Oslo. Photo: Wenche Gerhardsen / Oslo Cancer Cluster.
Testing in the clinic
A clinical pilot study at Vestre Viken breast centre has evaluated the impact of implementing population-based genetic testing strategy for breast cancer precision prevention. There were 80 study participants aged 40-50 who took the saliva-based PRS test at the breast centre. Some of these women were ultimately recommended earlier screening or more intensive screening.
“Half of them were recommended to participate in standard screening. Almost half of them were recommended to start screening at an earlier age than 50. One was recommended to start annual mammography screening immediately,” said Tone Hovda, senior radiologist at Vestre Viken.

Tone Hovda, senior radiologist at Vestre Viken. Photo: Sofia Linden / Oslo Cancer Cluster.
Is this cost-effective?
As with any innovation, the tests come at a price. Kari Kollstad, health economist at Oecona AS, has developed a cost-effectiveness analysis of a polygenic risk-tailored breast cancer screening program in Norway.
“The preliminary results show that risk-stratified screening is more costly than current mammography screening, mainly driven by: costs associated with implementing the test and consultations, as well as screening costs. Risk-stratified screening also resulted in an increase in life years and quality-adjusted life years, and a redistribution of cancer cases compared to current mammography screening,” said Kollstad.
This means that while the tests come with a cost, risk stratified screening means that breast cancer can be detected at an earlier stage and that patients live longer.

Kari Kollstad, health economist at Oecona AS. Photo: Sofia Linden / Oslo Cancer Cluster
Towards individual-based screening
The presentation was followed by a panel discussion about how to implement PRS tests in clinical practice.
“As an oncologist with 33 years of experience, I have encountered numerous cases of advanced breast cancer in women of various ages. When analyzing their risks and individual stories, I realized that we could prevent most of these unfortunate situations. Breast cancer risks vary significantly among women, but our screening approaches are the same for all. It is crucial that we enhance the current real-world practices for breast cancer prevention and screening, especially considering the availability of innovative solutions,” commented Dr. Peeter Padrik, CEO and Founder of Antegenes.
The company Antegenes has developed novel polygenic risk score-based genetic tests to estimate the risk of common cancers.

Peeter Padrik, CEO and founder of Antegenes. Photo: Sofia Linden / Oslo Cancer Cluster
“I believe precision cancer prevention will be the right way for the future. We need to see what we can do to find more women with breast cancer that need to be treated,” commented Ole Alexander Opdalshei, deputy secretary general, the Norwegian Cancer Society.
“We have been doing mammography screening for 30 years now and using the same procedures and equipment, so it is definitely time for change. We need to go more personalised. We need more efficient tools and we need to consider if it is time to extend the age range targeted in the program. I think the Antegenes test could contribute to making BreastScreen Norway more personalized and better for women: if we could start inviting women 48 years old, test all women and plan a personalised screening for the women. It would be expensive, but perhaps cost-effective in the long run,” commented Solveig Hofvind, Head of the Mammography Programme at The Cancer Registry of Norway.
- Read more about the AnteNOR project
- Please visit the Antegenes website to find out more about the PRS tests
Project partners: Antegenes, Oslo Cancer Cluster, Oslo University Hospital, University of Oslo, Vestre Viken.
This project is supported by the Norway Green ICT Programme.

 Wenche Gerhardsen
Wenche Gerhardsen






 Thomas London
Thomas London