Home testing to improve cancer prevention
Can home tests engage more people in cancer screening and save more lives?
“In Norway, 70% of all women are participating in the cervical cancer screening programme, which means 30% are not. Our goal is to include all and we need to get more women to participate,” said Sara Underland Mjelva, Leader of the Section for Prevention at the Norwegian Cancer Society.
This comment was made in a discussion about home testing during the webinar Results from the AnteNOR project: Norway’s way towards precision prevention at Oslo Cancer Cluster Innovation Park last week.
Reaching women at home
Home testing for HPV has been tested recently in Norway in a randomized clinical trial, led by Bo Terning Hansen, Senior Researcher at The Norwegian Institute of Public Health. The trial addressed women who hadn’t been screened for at least ten years.
“We found a huge difference in participation between the three control arms. Of those that just got the reminder letter, only 4% participated. While of those that received the test, 28% participated. That difference translates into a public health gain. We also found a huge difference in the diagnostic yield between the three arms,” explained Hansen.
This self-sampling device is now distributed by the Norwegian Cancer Registry and available in all GP offices in Norway. But what about other home tests?
Who pays for equal access?
Karl-Arne Johannessen, representing Tigeni, a company that offers home testing for cholesterol, long-term blood sugar, vitamins, and minerals, argued there are not enough financing solutions in Norway for home tests:
“If you go to the laboratory to take a test, the public healthcare pays for it, but there should also be public payment for the home tests in the future. It should be paid by the public if a doctor has asked you to take the test.”
Hansen agreed with Johannessen: “One thing is to get the tests funded, so everyone has equal access to them – that is the number one priority. There are also differences in ‘health literacy’ that you need to be aware of so you can compensate for that.”
“As a doctor myself, I support equal access to healthcare services. My experience is that currently public payers or healthcare organisations are quite conservative and cervical cancer is a good example. If we have a problem to engage individuals in preventive services, then home-based testing creates a more efficient additional option,” added Peeter Padrik, CEO of Antegenes, an Estonian healthcare company that develops PRS tests.
Predicting breast cancer
A PRS test is another kind of self-sampling device making headway in cancer screening. They are based on a technology called Polygenic Risk Score, which can provide a measure of someone’s personal risk to develop a disease. The Estonian-Norwegian collaboration project AnteNOR has for the last three years explored how to use these tests to improve prevention and early detection of breast cancer in Norway.

Peeter Padrik, CEO of Antegenes. Photo: Margit Selsjord/Oslo Cancer Cluster.
“The problem we are addressing is breast cancer, the most common cancer among women in Norway, Europe and worldwide. If we detect breast cancer as early as possible, then the treatment is very efficient,” said Padrik.
The breast cancer screening programme in Norway is for women aged 50-69, but 17% of breast cancer cases are among women younger than 50. It would not be reasonable to screen all women, so the challenge is to identify the younger women at risk.
Identifying genetic risk
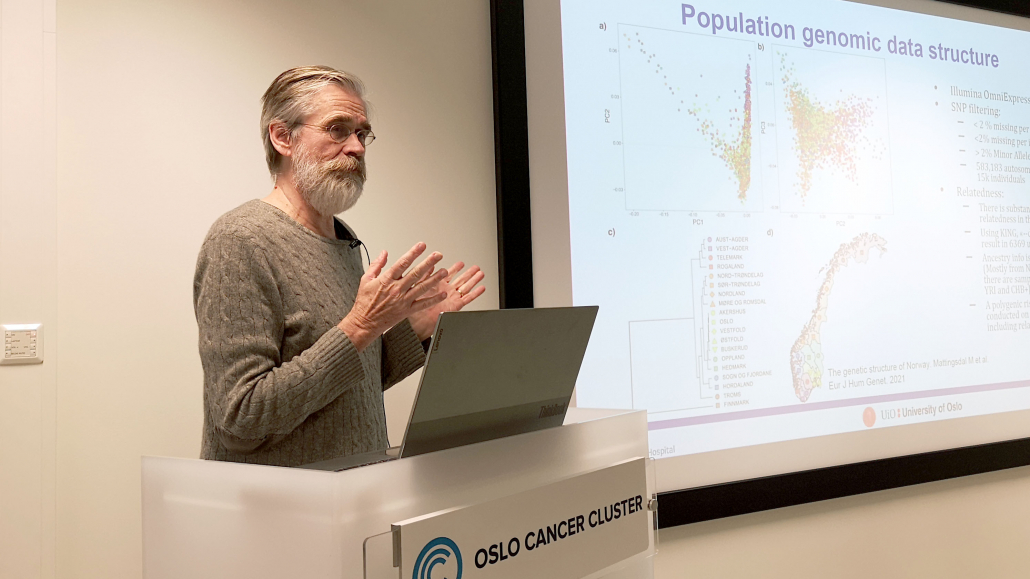
“The genetic susceptibility is a very strong associated factor to those who develop breast cancer,” said Eivind Hovig, Professor at the Department of Bioinformatics at the University of Oslo. Hovig has published a study looking at how a combination of genetic markers indicate Norwegian women’s personal risk of developing breast cancer.

Eivind Hovig, Professor at the Department of Bioinformatics at the University of Oslo. Photo: Margit Selsjord/Oslo Cancer Cluster.
“Polygenic risk score is becoming a complementary instrument for risk stratification for various cancers. We find indeed that we can identify that there are individuals that have high risk to develop breast cancer,” Hovig added.
- Read more in the article New research on genetic risk and breast cancer.
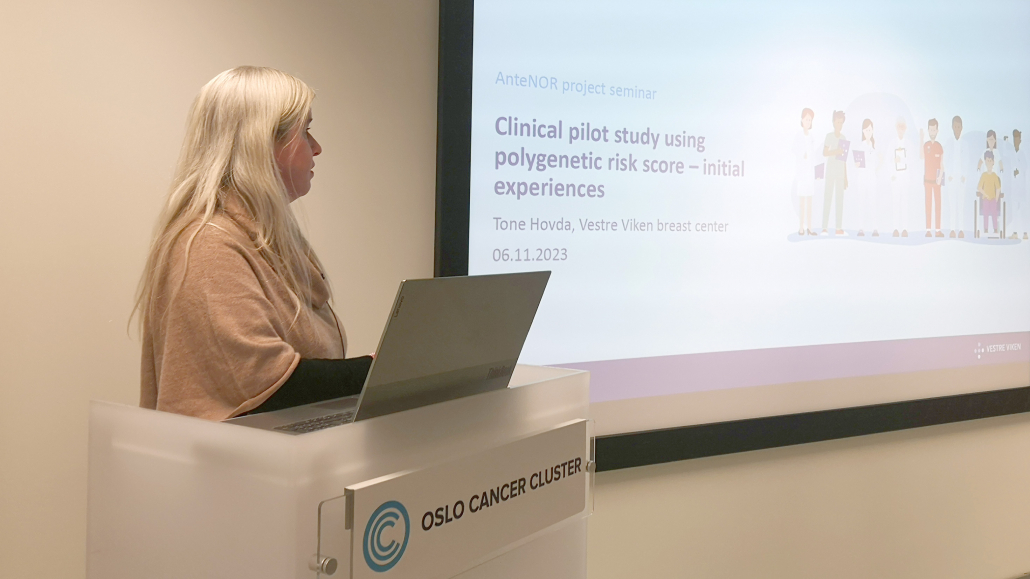
The potential of PRS as a tool for risk-based mammography screening was also explored in a clinical pilot as part of the AnteNOR project. In total, 80 women aged 40-50 years took the PRS test to find out their personal risk of developing breast cancer.

Tone Hovda, senior radiologist at Vestre Viken. Photo: Margit Seljord/Oslo Cancer Cluster
“40 women were recommended to participate in BreastScreen Norway. 39 women were recommended to start mammography every second year before the age of 50. Among them, six were recommended to start annual mammography later on. One woman was recommended to start annual mammography from now on,” said Tone Hovda, senior radiologist at Vestre Viken and lead investigator for the clinical pilot.
- Read more in the article Results from breast cancer screening pilot.
Of European importance
Genetic tests are also a political priority on the EU level, as early detection and diagnosis are now possible for an increasing number of cancers with underlying heritable genetic risk.
There is now a call for “Accessible and affordable tests to advance early detection of heritable cancers in the European regions”. The budget includes 10-12 million euros per proposal and the submission deadline is 18 September. 2024
Sofia Anderholm Strand, Senior Adviser at the Research Council of Norway, presented the call: “They stress the need to validate easy-to-use, affordable and accessible genetic tests for early detection of cancer.”
A special thank you to all AnteNOR project partners for their contributions.

The AnteNOR project has been funded by:



 Wenche Gerhardsen
Wenche Gerhardsen