Should Norway implement a clinical trial league table?
We asked four MBA students from Cambridge University to evaluate how patient recruitment practices in Norway can be improved.
The number of clinical trials in Norway has been declining over the last few years. There are many reasons behind this trend, but until now there have been few concrete solutions. With the number of cancer patients on the rise, there is a growing need for access to better treatments.
Oslo Cancer Cluster asked four students from Judge Business School at Cambridge University to research how the number of clinical trials in Norway can be improved. The students were Jacques Li, a doctor and entrepreneur from France; Diana Murguia Barrios, an economist and political scientist from Spain; Jason Yip, a chemistry engineer from England; and Sam Chong, a lawyer and economist from Malaysia and Australia.
“The number of clinical trials in Norway is less than half of the number in Denmark.”
The group focused on one of three factors that influence the number of clinical trials in Norway, namely: the patient recruitment practices. After a comparative analysis with other European countries, they came up with two main recommendations on how Norway can improve patient recruitment.

How do we motivate hospitals and doctors to recruit more patients to clinical trials?
One: Motivating hospitals
The group compared patient recruitment in Norway to France, United Kingdom and USA. Norway was the only country where hospitals don’t have any non-financial incentives to recruit patients to clinical trials. If a hospital’s reputation could be improved in a concrete way by having clinical trials, patient recruitment could also be improved.
The group proposed to create a league table for all hospitals, with cancer trial participation as one of the metrics. This would create competition between hospitals, encourage collaboration between smaller hospitals and larger ones, and make information about clinical trials accessible to patients.
“If hospitals were ranked against each other based on clinical trial output, they would more actively recruit into trials due to the reputational incentive.”
The group also uncovered a misalignment between the funding source and the implementers of the clinical trials. Funding is passed from the Norwegian Health Ministry to the regional health authorities, instead of directly to the hospitals who conduct the trials. The group recommended that the hospitals need direct financial incentives to conduct the trials.
“Regional health authorities in Norway need to ensure that funding provided to them for research is passed down to the hospitals conducting clinical trials.”

How do we raise awareness among patients and doctors about clinical trial participation?
Two: Raising awareness
A second discovery in the report was the lack of awareness about clinical trials among both patients and doctors. Patients in Norway lack access to relevant information that would empower them to opt into clinical trials. There was similarly a lack of exposure to clinical trials among early career doctors and a lack of initiatives to collaborate on clinical trials among advanced career doctors.
“Raising awareness among stakeholders is key to improve clinical trial recruitment.”
The students suggested working in partnership with patient organisations to raise awareness among patients. They recommended a national awareness campaign to inform where patients can find up-to-date information about clinical trials. All hospitals could keep lists of their ongoing clinical trials available on their websites.
“If patients knew the benefits of clinical research, they would select a hospital that is ranked highly.”
The group also provided recommendations to raise awareness among doctors to work on clinical trials. Rotational programs and supplementary courses on research methods and clinical trials may spark interest among medical students to pursue work in clinical trials. Seminars and workshops can help to both raise awareness and inspire collaborative efforts among doctors in their advanced careers.
Oslo Cancer Cluster wishes to extend a big thank you to everyone who agreed to be interviewed for this research project:
- Ali Areffard, Medical team, Bristol Myers Squibb
- Øyvind Arnesen, Chairman of the Board, Oslo Cancer Cluster
- Siri Kolle, Vice President Clinical, Inven2
- Jónas Einarsson, former Chairman of the Board of Oslo Cancer Cluster and one of the founders of Oslo Cancer Cluster Innovation Park
- Maiken Engelstad, Deputy Director, Ministry of Health and Care Services
- Katrine Bryne, Senior Advisor, Legemiddelindustrien (LMI)
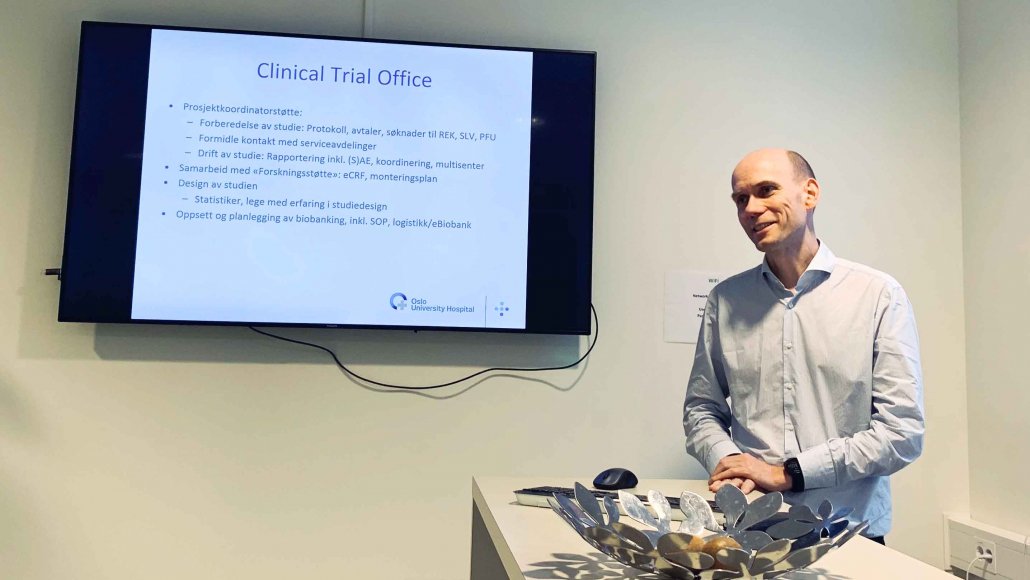
- Kristin Bjordal, Business Manager for Research Support and Research Manager in Oslo Hospital Service (OSS) and Chairman of the Board of NorCrin
- Ida Kommandtvoll, Advisor, Department of Strategy and Analysis, The Norwegian Cancer Society
- Knut Martin Torgersen and medical team, Merck
- Steinar Aamdal, the founder of The Clinical Trial Department, Oslo University Hospital
View and download the following PDF of the Cambridge report to learn more.
Note: This is a short version of the report, the fuller version also includes an Appendix containing detailed information about all the underlying data and interview material. Please get in touch with Communications Adviser Sofia Lindén if you are interested in reading the full Appendix.
 Loading...
Loading...